Introduction
Vitamin D, often referred to as the “sunshine vitamin,” plays a crucial role in maintaining overall health. It is a fat-soluble vitamin that helps the body absorb calcium and phosphorus, which are essential for strong bones and teeth. Beyond its role in bone health, vitamin D is vital for a well-functioning immune system, muscle strength, and even mental health. Despite its importance, vitamin D deficiency is one of the most common nutrient deficiencies worldwide.
Statistics show that approximately 1 billion people globally suffer from vitamin D deficiency, with nearly 50% of the population having insufficient levels of this vital nutrient. Factors such as limited sun exposure, darker skin tones, aging, and dietary restrictions contribute to this widespread problem. In countries with long winters or limited sunlight, the prevalence of deficiency is even higher. According to a study published in The Journal of Clinical Endocrinology & Metabolism, up to 42% of adults in the United States have vitamin D deficiency, and similar trends are observed in Europe and other parts of the world.
The purpose of this article is to help readers recognize the common signs and symptoms of vitamin D deficiency. Many individuals remain unaware that their fatigue, bone pain, or even frequent illnesses could be linked to low vitamin D levels. By understanding these signs, you can take proactive steps to address the deficiency and improve your overall health. Whether through diet, supplements, or lifestyle changes, identifying the warning signs early can make a significant difference in maintaining your well-being.
1. Persistent Fatigue and Low Energy Levels
One of the earliest and most common signs of vitamin D deficiency is persistent fatigue and low energy levels. While occasional tiredness is a normal part of life, chronic fatigue that doesn’t improve with rest may point to an underlying issue, such as a lack of vitamin D.
Vitamin D plays an essential role in energy production by helping regulate calcium and phosphate levels in the body. These minerals are critical for muscle function and cellular energy production. A deficiency in vitamin D can lead to impaired mitochondrial function—the powerhouse of the cell—which reduces the energy available to your body, leaving you feeling sluggish and drained.
Research supports the connection between low vitamin D levels and fatigue. For instance, a study published in North American Journal of Medical Sciences found that individuals with vitamin D deficiency often reported fatigue as a primary complaint. After correcting their deficiency through supplementation, many participants experienced a significant improvement in energy levels. Another study in Medicine (Baltimore) observed that patients with low vitamin D levels experienced fatigue more frequently than those with normal levels, highlighting a clear link between the two.
Chronic tiredness due to vitamin D deficiency is often misattributed to stress, lack of sleep, or other health conditions, making it important to identify this symptom correctly. If you find yourself constantly feeling tired despite adequate rest, consulting a healthcare professional for a vitamin D blood test could help uncover the root cause. Correcting a deficiency not only boosts energy but also contributes to overall vitality and well-being.
2. Bone Pain and Weakness
Vitamin D is essential for maintaining strong, healthy bones because it facilitates the absorption of calcium and phosphorus—two minerals crucial for bone density and structure. When the body is deficient in vitamin D, it struggles to absorb enough calcium from the diet, forcing it to pull calcium from the bones to maintain blood levels. Over time, this can lead to bone pain, weakness, and a higher risk of fractures.
One of the earliest and most noticeable symptoms of vitamin D deficiency is dull, aching pain in the bones, particularly in the lower back, hips, legs, and ribs. This discomfort may worsen during activities that put stress on the bones, such as walking or lifting. If left unaddressed, chronic vitamin D deficiency can lead to more severe conditions like osteomalacia (softening of bones) in adults or rickets in children. Both conditions are characterized by weakened bones that are prone to fractures and deformities.
Additionally, long-term vitamin D deficiency is a significant contributor to osteoporosis, a condition where bones become brittle and porous, increasing the risk of fractures even from minor falls or injuries. Osteoporosis is especially prevalent in older adults and postmenopausal women, partly due to reduced vitamin D levels with age.
Clinical studies highlight this connection between vitamin D and bone health. A review in The Journal of Clinical Endocrinology & Metabolism found that individuals with vitamin D deficiency were at a much higher risk of fractures and bone-related disorders. Furthermore, supplementation with vitamin D has been shown to reduce the likelihood of fractures and improve bone density, especially when combined with calcium.
If you’re experiencing persistent bone pain or find yourself unusually prone to fractures, it could be a sign of insufficient vitamin D. Addressing this deficiency early through dietary changes, safe sun exposure, or supplements can help protect your bones and maintain their strength as you age.
3. Frequent Illness or Infections
Vitamin D plays a pivotal role in supporting the immune system, acting as a vital defense mechanism against infections and illnesses. It helps the body produce and activate antimicrobial peptides, such as cathelicidin, which have the ability to fight off harmful pathogens like bacteria and viruses. Without sufficient vitamin D, the immune system may become compromised, making it easier for infections to take hold.
One of the most noticeable signs of a vitamin D deficiency is experiencing frequent colds, flu, or respiratory infections. Studies have shown that individuals with low vitamin D levels are more likely to develop upper respiratory tract infections, such as bronchitis and pneumonia. For instance, research published in BMJ found that vitamin D supplementation reduced the risk of acute respiratory infections, particularly in individuals with existing low levels.
Vitamin D also plays a role in regulating immune responses to prevent excessive inflammation. Deficiency can lead to a weaker immune system that not only struggles to fight infections but also reacts poorly, potentially causing more harm than good. This is particularly concerning during seasonal changes when colds and flu are more prevalent.
For those frequently battling illnesses, boosting vitamin D levels through diet, supplementation, or sunlight exposure can help fortify the immune system. Foods rich in vitamin D, such as fatty fish, egg yolks, and fortified products, can be excellent sources. In cases where natural intake is insufficient, supplements are a safe and effective way to maintain adequate levels, especially during winter months when sunlight exposure is limited.
If you find yourself constantly falling sick, it may be worth checking your vitamin D levels. Addressing a deficiency could not only strengthen your immune system but also improve your overall resilience to infections.
4. Muscle Weakness and Cramps
Vitamin D plays an important role in maintaining proper muscle function and strength. It supports muscle health by facilitating calcium absorption, which is essential for muscle contractions, and by directly influencing muscle cell growth and repair. When vitamin D levels are low, the muscles may struggle to function optimally, leading to weakness and discomfort.
A common symptom of vitamin D deficiency is muscle weakness, which may feel like an inability to perform physical tasks that were previously manageable. This can manifest as difficulty climbing stairs, lifting objects, or even maintaining balance. Muscle weakness associated with vitamin D deficiency is particularly noticeable in the elderly, where it significantly increases the risk of falls and injuries.
Another frequent symptom is muscle cramps or spasms, which can occur because of disrupted calcium metabolism. Calcium is crucial for normal muscle contractions, and without adequate vitamin D to regulate calcium levels, the muscles may contract improperly, leading to painful cramps or twitching. This issue is often most apparent in the legs or feet, especially at night.
Studies highlight the connection between vitamin D levels and muscle health. Research published in The Journal of Clinical Endocrinology & Metabolism found that individuals with sufficient vitamin D had better muscle strength and function compared to those with a deficiency. Another study showed that vitamin D supplementation in deficient individuals led to significant improvements in muscle performance and reduced cramping.
If you’re experiencing frequent muscle weakness or cramps, it could be a sign of insufficient vitamin D. Incorporating vitamin D-rich foods into your diet, such as salmon, mackerel, or fortified milk, along with regular sun exposure, can help restore levels and improve muscle health. Supplements are also a practical option, especially for those with limited sun exposure or dietary restrictions.
5. Mood Changes, Including Depression
Vitamin D plays a critical role in regulating mood and emotional well-being, largely due to its influence on serotonin, a neurotransmitter that helps stabilize mood and promote feelings of happiness. Often referred to as the “sunshine vitamin,” vitamin D is produced in the body when exposed to sunlight. A deficiency in vitamin D can disrupt serotonin production, potentially leading to mood changes and symptoms of depression.
Research has shown a strong association between low vitamin D levels and an increased risk of depression. One study published in The British Journal of Psychiatry found that individuals with vitamin D deficiency were more likely to experience depressive symptoms than those with adequate levels. This connection is particularly evident during the winter months, when reduced sunlight exposure can lead to a condition known as seasonal affective disorder (SAD)—a type of depression linked to a lack of sunlight.
Symptoms of depression caused by vitamin D deficiency may include feelings of sadness, fatigue, irritability, and a general lack of motivation. For some individuals, these mood changes may be subtle, while for others, they can significantly impact daily life.
Vitamin D supplementation has shown promise as a supportive treatment for individuals struggling with depression. Studies have indicated that increasing vitamin D intake can improve mood, particularly in those who were deficient to begin with. For example, a study in The Journal of Post-Acute and Long-Term Care Medicine found that vitamin D supplementation reduced depressive symptoms in older adults with low vitamin D levels.
To support mental health and mood stability, aim to maintain optimal vitamin D levels through regular sun exposure, a diet rich in vitamin D (such as fatty fish, egg yolks, and fortified foods), or supplements if needed. If you’re experiencing persistent mood changes or depression, it’s also important to consult a healthcare provider to explore underlying causes and appropriate treatment options.
6. Hair Thinning or Hair Loss
Vitamin D plays a vital role in maintaining healthy hair by supporting hair follicle health and regulating the hair growth cycle. Hair follicles are tiny structures in the scalp that produce hair, and they contain vitamin D receptors that are crucial for stimulating new growth. When vitamin D levels are insufficient, the hair follicle’s ability to produce and maintain hair may be compromised, leading to hair thinning or loss.
A prolonged vitamin D deficiency can disrupt the hair follicle’s natural growth cycle, particularly the anagen phase, which is the active growth phase. This disruption may cause hair follicles to enter a resting state, resulting in reduced hair production and increased shedding. While occasional hair shedding is normal, persistent thinning could be an indicator of an underlying vitamin D deficiency.
Scientific studies have highlighted the connection between vitamin D deficiency and conditions like alopecia areata, an autoimmune disorder that causes patchy hair loss. Research published in the Journal of Clinical and Diagnostic Research showed that individuals with hair loss often have lower serum vitamin D levels compared to those without hair loss. While vitamin D deficiency alone may not directly cause conditions like male or female pattern baldness, it can exacerbate hair loss in individuals who are already predisposed to it.
To prevent or address hair thinning caused by vitamin D deficiency:
- Dietary intake: Include vitamin D-rich foods like fatty fish, fortified dairy products, and egg yolks in your meals.
- Sun exposure: Aim for 10–30 minutes of sunlight exposure several times a week to naturally boost vitamin D production.
- Supplements: Consider vitamin D supplements, particularly if you have limited sun exposure or dietary restrictions.
If you’re experiencing significant hair thinning or hair loss, it’s important to consult a healthcare provider. They can assess your vitamin D levels and determine whether supplementation or additional treatments are needed to restore healthy hair growth.
7. Slow Wound Healing
Vitamin D is essential for the body’s inflammatory response and tissue repair, both of which play a crucial role in wound healing. When the body sustains an injury, vitamin D helps regulate the immune system and promote the production of compounds, such as antimicrobial peptides, that prevent infection. Additionally, vitamin D aids in tissue regeneration by supporting the growth and differentiation of skin cells that are necessary for repairing damaged tissue.
A deficiency in vitamin D can impair these processes, leading to delayed wound healing after injuries, surgeries, or minor skin abrasions. For example, individuals with low vitamin D levels may notice that cuts or bruises take longer to close and heal, leaving the affected area more vulnerable to infection and scarring.
Research has demonstrated the connection between vitamin D and wound healing. A study published in the Journal of Investigative Dermatology found that vitamin D supplementation improved the healing of chronic wounds, such as diabetic foot ulcers, by enhancing the immune response and tissue repair. Similarly, individuals recovering from surgeries with optimal vitamin D levels have been shown to experience faster and more effective healing compared to those who are deficient.
If you notice slow healing of wounds or recurrent infections at injury sites, it might be worth checking your vitamin D levels. Boosting your vitamin D intake can support the body’s natural healing process through:
- Sunlight exposure: Promotes vitamin D synthesis for faster tissue repair.
- Dietary sources: Foods rich in vitamin D, like salmon, tuna, and fortified products, help maintain sufficient levels.
- Supplements: High-quality vitamin D supplements can provide additional support for those with chronic deficiencies.
While vitamin D can be a key factor in wound healing, slow recovery may also stem from other issues, such as poor circulation, diabetes, or nutritional deficiencies. If delayed healing persists, consult a healthcare provider for a comprehensive evaluation.
8. Bone Deformities in Children (RicketS)
Rickets is a bone disorder caused by a deficiency in vitamin D, which is essential for calcium absorption and bone development. In children, this can lead to noticeable skeletal deformities such as bowed legs, knock-knees, and a curved spine. These deformities occur because the bones become soft and weak due to insufficient vitamin D, making them unable to support the child’s weight properly. Other signs of rickets include delayed growth, muscle weakness, and bone pain, which can limit a child’s mobility and overall development.
Vitamin D plays a crucial role in childhood development by helping the body absorb calcium, which is vital for strong bones. Without adequate vitamin D, children’s bones can become poorly mineralized, leading to deformities like those seen in rickets. In addition to bone health, vitamin D also supports muscle function and the immune system, making it essential for a child’s overall growth and well-being. Ensuring children receive enough vitamin D through sunlight, diet, or supplements is key to preventing rickets and supporting their long-term health.
Cognitive Issues or “Brain Fog” and the Role of Vitamin D
Vitamin D, commonly associated with bone health, plays a vital role in brain function as well. Recent research has shown that low vitamin D levels can impair memory, focus, and overall cognitive function. Known colloquially as “brain fog,” these cognitive issues can manifest as difficulty concentrating, feeling mentally sluggish, or experiencing forgetfulness. These symptoms are often subtle but can significantly impact daily life, leading to frustration and decreased productivity.
Studies have shown a direct correlation between low vitamin D levels and cognitive decline. The brain’s vitamin D receptors are involved in various processes such as neurogenesis (the formation of new neurons) and synaptic plasticity (the ability of the brain to adapt and form new connections). When vitamin D is insufficient, these processes may be impaired, leading to difficulties in learning, memory retention, and even mood regulation. In older adults, this can result in noticeable cognitive decline, often associated with conditions like Alzheimer’s disease and other forms of dementia.
One significant concern is the link between vitamin D deficiency and an increased risk of developing dementia. Several large studies have found that individuals with low levels of vitamin D are at a higher risk of developing cognitive impairments as they age. In fact, those with severe deficiencies may experience an accelerated decline in brain function. While vitamin D alone is not the sole cause of dementia, its deficiency appears to contribute to the onset or progression of cognitive decline, particularly in older adults.
The connection between vitamin D and cognitive health is also evident in mental health disorders. Low vitamin D levels have been linked to depression, anxiety, and mood disturbances. Inadequate vitamin D may affect the brain’s ability to regulate serotonin, a neurotransmitter that plays a key role in mood and cognitive function. As serotonin levels fluctuate, so too can cognitive abilities and emotional well-being, potentially leading to feelings of confusion, irritability, and low motivation.
Fortunately, improving vitamin D levels can have a positive impact on cognitive function. Research suggests that supplementing vitamin D in individuals with deficiencies can lead to improvements in memory, focus, and overall brain health. For those at risk of dementia or cognitive decline, ensuring adequate vitamin D intake through sunlight, dietary sources, or supplements can serve as a protective measure. In fact, some studies have shown that individuals who maintain optimal vitamin D levels throughout their lives may experience slower rates of cognitive decline and a reduced risk of developing dementia-related diseases.
While vitamin D supplementation can help improve cognitive function in deficient individuals, it’s important to note that it is not a cure-all. Cognitive issues often result from a complex mix of factors, including genetics, lifestyle, and environmental influences. Nonetheless, ensuring sufficient vitamin D levels is a relatively simple and effective strategy to support brain health and reduce the risk of cognitive impairments as we age.
In conclusion, vitamin D is essential not only for bone health but also for maintaining proper cognitive function. Low levels of vitamin D can lead to brain fog, memory issues, and an increased risk of dementia. By recognizing the importance of vitamin D in brain health and taking steps to maintain adequate levels, individuals can improve cognitive function and potentially prevent the onset of more severe cognitive conditions in the future.
Increased Risk of Chronic Conditions: The Impact of Vitamin D Deficiency
Vitamin D is a crucial nutrient that supports many functions in the body, from bone health to immune system regulation. However, insufficient levels of vitamin D over an extended period can have serious long-term effects, increasing the risk of several chronic conditions. These include hypertension, heart disease, and type 2 diabetes, all of which are linked to vitamin D deficiency in various studies. Understanding how low vitamin D levels can exacerbate these conditions is key to recognizing the importance of maintaining adequate vitamin D levels for overall health.
One of the most concerning long-term effects of vitamin D deficiency is its contribution to hypertension or high blood pressure. Vitamin D helps regulate blood pressure by influencing the renin-angiotensin system, which controls the contraction and relaxation of blood vessels. When vitamin D levels are low, this system becomes dysregulated, leading to increased resistance in blood vessels and higher blood pressure. Studies have shown that individuals with low vitamin D are more likely to develop hypertension, and supplementing with vitamin D may help lower blood pressure in those with deficiency.
In addition to hypertension, vitamin D deficiency has been linked to heart disease. Vitamin D plays a role in regulating inflammation and protecting blood vessels from damage. When levels are insufficient, inflammation in the body can rise, contributing to the development of atherosclerosis—the buildup of plaque in the arteries, which is a major risk factor for heart disease. Low vitamin D is also associated with higher levels of LDL (“bad”) cholesterol, which can further increase the risk of heart attack and stroke. Some studies suggest that correcting vitamin D deficiency may help reduce the risk of cardiovascular events, although more research is needed to fully understand the relationship between vitamin D and heart health.
Another chronic condition that is exacerbated by vitamin D deficiency is type 2 diabetes. Vitamin D plays a role in the body’s ability to regulate insulin production and glucose metabolism. Insulin resistance, a hallmark of type 2 diabetes, is more likely to develop when vitamin D levels are low. Several studies have found that individuals with insufficient vitamin D are at a higher risk of developing type 2 diabetes, particularly in those with obesity, who tend to have lower vitamin D levels. Ensuring adequate vitamin D intake may help improve insulin sensitivity and lower the risk of developing diabetes.
The relationship between vitamin D and chronic conditions like hypertension, heart disease, and type 2 diabetes highlights the importance of maintaining optimal levels of the vitamin throughout life. A deficiency in vitamin D doesn’t just affect bone health but can also contribute to systemic inflammation, impaired immune function, and metabolic disturbances that increase the risk of these chronic conditions. Therefore, ensuring adequate vitamin D intake through sunlight, diet, or supplementation can be an essential part of managing and preventing long-term health issues.
In conclusion, vitamin D deficiency is not just a concern for bone health but is also linked to several chronic conditions, including hypertension, heart disease, and type 2 diabetes. By maintaining sufficient vitamin D levels, individuals can help reduce their risk of developing these serious health conditions and improve their overall well-being. Regular screening, proper nutrition, and appropriate supplementation can go a long way in preventing the negative effects of vitamin D deficiency on long-term health.
9. How to Test for Vitamin D Deficiency
Vitamin D is an essential nutrient that plays a key role in many bodily functions, but its deficiency is often difficult to detect based on symptoms alone. Since vitamin D is vital for bone health, immune function, and more, it’s important to understand how to test for a deficiency and when to seek professional advice. Here, we’ll explore the common methods used to test for vitamin D deficiency and provide guidance on when it’s time to consult a healthcare provider.
Common Methods for Testing Vitamin D Levels
The most accurate and commonly used method for diagnosing vitamin D deficiency is through a blood test that measures the levels of 25-hydroxyvitamin D (25(OH)D) in the bloodstream. This form of vitamin D is the primary circulating form and reflects the total amount of vitamin D your body has stored. The test is relatively simple, requiring a blood draw, and is typically performed at a healthcare facility, although at-home testing kits are also available for convenience.
The results from this test are generally reported in nanograms per milliliter (ng/mL), with the following general guidelines for vitamin D status:
- Deficient: Below 20 ng/mL
- Insufficient: 20-29 ng/mL
- Sufficient: 30-50 ng/mL
- Toxic: Above 100 ng/mL (although toxicity is rare, it can occur with excessive supplementation)
If your results show that your vitamin D levels are low, your healthcare provider will likely recommend a course of action to address the deficiency, such as dietary changes, increased sun exposure, or vitamin D supplementation.
When to Consult a Healthcare Provider
You may want to consider testing for vitamin D deficiency if you have risk factors that make you more susceptible to low levels of this nutrient. Risk factors include living in areas with limited sunlight, having darker skin (which reduces the body’s ability to produce vitamin D from sunlight), being elderly, having certain medical conditions (like osteoporosis, obesity, or digestive disorders), or taking medications that affect vitamin D metabolism.
It’s also advisable to consult a healthcare provider if you experience symptoms that may indicate a deficiency, such as fatigue, muscle weakness, bone pain, or frequent infections. However, it’s important to note that these symptoms can be caused by various conditions, so testing is necessary to confirm whether vitamin D deficiency is the underlying cause.
If you are at risk for vitamin D deficiency or have experienced any of these symptoms, a simple blood test can provide the clarity you need. Your healthcare provider will interpret the results and guide you on the best course of action to correct any deficiencies. This might include increasing your intake of vitamin D-rich foods (like fatty fish, fortified dairy, and eggs), taking supplements, or ensuring that you get more sunlight exposure. It’s always important to follow medical advice to avoid self-diagnosing and potentially mismanaging your health.
10. Sources of Vitamin D
Vitamin D is a unique nutrient in that it can be obtained through various sources, both natural and fortified, which are essential for maintaining optimal health. While it’s often referred to as the “sunshine vitamin,” vitamin D can be found in certain foods and supplements, which is especially important for those at risk of deficiency. Let’s explore the natural sources of vitamin D and the importance of supplementation for individuals who may have difficulty getting enough from these sources.
Natural Sources of Vitamin D
One of the most efficient ways to obtain vitamin D is through sunlight. When your skin is exposed to UVB rays from the sun, it produces vitamin D. For most people, spending about 10-30 minutes in the sun several times a week can provide enough vitamin D. However, this can vary based on factors like geographic location, skin color, age, and time of year. People with darker skin or those living in northern latitudes, where sunlight is limited during the winter months, may have a harder time synthesizing adequate amounts of vitamin D.
In addition to sunlight, certain foods can help boost your vitamin D intake. Fatty fish such as salmon, mackerel, sardines, and tuna are among the best natural sources, providing high amounts of vitamin D in each serving. A single serving of fatty fish can contain more than the daily recommended amount of vitamin D, making it an excellent choice for those looking to support their health.
Egg yolks are another natural source of vitamin D, though they provide less than fatty fish. One large egg yolk typically contains around 40 IU (international units) of vitamin D, which can contribute to your daily intake, especially when consumed as part of a balanced diet. However, it’s important to note that egg whites do not contain vitamin D, so whole eggs are necessary to reap this benefit.
Fortified foods are an essential source of vitamin D for many individuals, as it can be difficult to obtain adequate levels from food alone. Common foods that are fortified with vitamin D include milk, orange juice, and breakfast cereals. Fortification helps ensure that people who may not consume fatty fish or have limited sun exposure can still meet their vitamin D needs through their diet. In some cases, plant-based milk alternatives, such as soy or almond milk, are also fortified with vitamin D, making them an excellent option for vegans and those who are lactose intolerant.
Importance of Supplementation for Those at Risk of Deficiency
While natural sources of vitamin D are important, supplementation can be crucial for individuals who are at a higher risk of deficiency. This includes people who live in areas with limited sunlight, have darker skin, are elderly, or have certain health conditions that impair vitamin D absorption, such as Crohn’s disease or celiac disease. Additionally, people who follow vegan diets may struggle to obtain enough vitamin D from food sources alone, as most natural sources of the vitamin are animal-based.
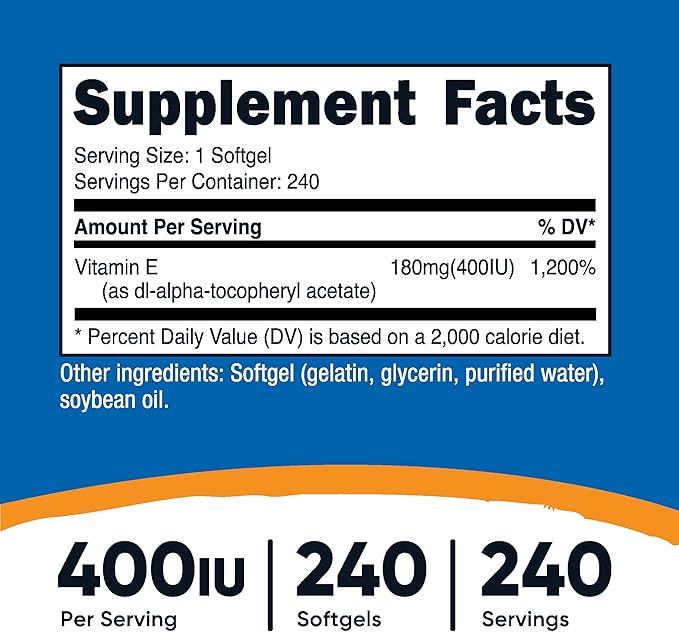
For individuals who are unable to get sufficient vitamin D from sunlight and diet, taking a vitamin D supplement can help fill the gap. Supplements are available in two main forms: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin D3 is generally considered more effective at raising vitamin D levels in the body, as it is the form produced by the skin in response to sunlight.
Consulting a healthcare provider is important before starting supplementation, as excessive vitamin D intake can lead to toxicity. While deficiency is a common issue, too much vitamin D can lead to problems such as kidney damage, calcium buildup in the blood, and bone loss. Your healthcare provider can help determine the appropriate dosage based on your individual needs and risk factors.
Sources
- National Institutes of Health (NIH) Vitamin D Fact Sheet.
- Studies from The Journal of Clinical Endocrinology & Metabolism.
- Research published in The American Journal of Clinical Nutrition.
- Mayo Clinic resources on vitamin D deficiency.
- World Health Organization (WHO) reports on global vitamin D deficiency rates.